The how long to wait for sex after yeast infection treatment question deserves a straight answer you can trust. Short version: finish the full course, wait until all symptoms are gone, and give your body a little extra time to settle before you get intimate again. That usually means several days after your last dose, but the exact timing depends on your treatment (topical cream/suppository vs. oral pill), your symptoms, and your comfort. Below, you’ll find a simple, step-by-step way to decide when it’s safe—plus key tips to prevent reinfection, protect condoms, and keep tissues from getting re-irritated.
The simple rule of three: finish, symptom-free, buffer
1) Finish treatment.
Complete every dose—even if you feel better early. Stopping mid-course is a common reason symptoms rebound. Clinical guidance notes that short-course azole therapies (1–7 days) are effective when taken exactly as directed. CDC
2) Be 100% symptom-free.
No itching, burning, soreness, swelling, or clumpy discharge. If any symptom lingers, you’re not “cleared” yet. Sex too soon can prolong healing, increase irritation, and contribute to ping-pong reinfection. Medical News Today
3) Add a short buffer.
Give tissues time to calm after the last dose—especially after topical products. Many people do well waiting 2–3 days beyond “last dose + symptom-free.” If you took a single-dose pill, many clinicians suggest avoiding sex for about a week while things resolve. (Details below.) ACOG+1
Why waiting matters (and not just for you)
- Reduces reinfection risk. Candida can pass via close sexual contact. If sex happens mid-treatment or during a flare, partners can trade the infection back and forth. Medical News Today
- Protects healing tissue. Inflamed mucosa is sensitive; friction can worsen symptoms or trigger microtears.
- Prevents condom failure. Many vaginal creams/suppositories are oil-based and can weaken latex condoms and diaphragms during treatment (and sometimes shortly after). That’s a real, documented interaction. CDC+2nhs.uk+2
How long to wait by treatment type
If you used an OTC or prescription vaginal azole (cream, suppository, ovule)
- Finish the labeled course (1-, 3-, 7- or 14-day regimens).
- Stay abstinent until symptoms are gone, then add a 2–3 day buffer after the last dose before any penetration or vigorous external play.
- Condom note: Because these products are often oil-based, do not rely on latex condoms/diaphragms during treatment; check the label for the specific time window and consider avoiding latex barriers for a few days after the final dose, or use non-latex alternatives (polyurethane/polyisoprene) during that window. CDC+1
If you took oral fluconazole (single 150-mg pill or multi-dose plan)
- Symptoms often start improving within 24–72 hours and may take a few days to fully resolve. GoodRx+1
- Plan to wait until you’re symptom-free and give it about a week from the dose before resuming sex, unless your clinician advised otherwise (some need longer if symptoms were severe). ACOG
If symptoms persist past 3 days after fluconazole—or return within weeks—check in with a clinician. Recurrent or non-albicans infections often need a different plan. CDC
A practical yes/no checklist before you resume sex
- Have I completed every dose?
- Are itching, burning, soreness, swelling, and discharge completely gone?
- Has it been at least 48–72 hours since my last vaginal dose, or about a week since a single oral dose, with no symptoms?
- If we use condoms, am I outside the window where oil-based azoles weaken latex (or using a non-latex condom)? CDC+1
- Do I feel safe and comfortable saying “slow,” “softer,” or “stop”?
If any answer is “no,” give it more time.
Protecting condoms and your contraception
- Oil + latex don’t mix. Many intravaginal azoles can damage latex condoms and diaphragms during treatment; some labels caution you to avoid latex barriers for a period after treatment, too. Read your specific product insert. CDC+1
- Workarounds: Use non-latex condoms (polyurethane/polyisoprene), abstain until you’re past the caution window, or plan non-penetrative intimacy.
- Hormonal birth control isn’t affected by clotrimazole/miconazole creams; still, confirm with your pharmacist if you’re on other meds. nhs.uk
Comfort-first tips when you’re ready to be intimate again
- Start slow. First time back, keep things gentle and short.
- Use plenty of water-based lube. It reduces friction on recently healed tissue (and is condom-compatible).
- Favor stable positions with easy angle control and shorter strokes; avoid anything that pulls or rubs the vulva.
- Pause at the first hint of burning or dryness. That’s feedback, not failure—take a break and reassess tomorrow.
- Consider non-penetrative play the first night back (kissing, massage, cuddling, hand-holding, mutual touch over underwear).
What about oral sex?
Yeast infections aren’t classic STIs, but oral–genital contact can play a role in some cases. If your mouth/throat or partner’s genitals are symptomatic, avoid contact until cleared. Restart oral only when everyone is symptom-free and you’re past treatment windows. Mayo Clinic
Do partners need treatment?
For uncomplicated vulvovaginal candidiasis, routine partner therapy isn’t recommended. If a male partner has symptoms of balanitis (itching, redness on the glans), they should be evaluated and may benefit from topical antifungals. For recurrent or complicated cases, follow a clinician’s plan. CDC
When to call a clinician (don’t wait it out)
- Symptoms don’t improve within 72 hours of starting treatment.
- Symptoms return within 2 months (possible recurrence or wrong diagnosis). CDC
- You’ve had ≥3 infections in <12 months (recurrent VVC often needs longer therapy or cultures to check species/resistance). CDC
- You’re pregnant, immunocompromised, or have poorly controlled diabetes—treatment approaches differ. CDC
- You’re unsure it’s yeast (BV, trichomoniasis, and dermatitis can look similar—testing matters).
A gentle, step-by-step timeline you can copy
Day 0–1: Start treatment. Avoid sex. Use breathable cotton underwear; keep the area dry; skip tight leggings.
Day 2–3: If using a single-dose oral pill, you may start feeling relief now; if using a 3- or 7-day cream, keep dosing nightly. Still no sex; protect condoms from oil-based products. GoodRx+1
Day 4–7: Symptoms fade. Finish every dose. Hydrate. Avoid douching or scented soaps (they irritate tissue and can worsen vaginitis). ACOG
48–72 hours after final vaginal dose (or ~1 week after oral dose): If you’re truly symptom-free, consider gentle, shorter sessions with lots of lube—or choose cozy, non-penetrative intimacy first night back. ACOG
If anything stings or burns, stop immediately, rinse with lukewarm water, and try again in a few days.
Smart prevention habits once you’re healed
- Finish antibiotics with a plan. If you need systemic antibiotics in the future, ask your clinician about yeast-prevention strategies. ACOG
- Skip douching and fragranced washes; the vagina is self-cleaning. ACOG
- Air out post-workout. Change damp clothes quickly; choose breathable underwear.
- Manage underlying factors. Good glucose control if you have diabetes; discuss immunosuppressants with your doctor if yeast recurs. CDC
- If infections recur, ask about culture-guided therapy or longer regimens; some cases need multi-dose fluconazole or 7–14 days of topical therapy before maintenance. CDC
What to do instead while you wait
Healing time doesn’t have to mean “no intimacy.” Try:
- Cuddle rituals: forehead-to-forehead breathing for one minute.
- Massage over clothing: shoulders, neck, hands, and feet with unscented lotion.
- Kissing + compliments: one specific praise, every minute for ten minutes.
- External, non-friction touch: thighs and back with a soft blanket between skin if you’re sensitive.
- Simple sensory play: warm towel on shoulders, soft music, dim light.
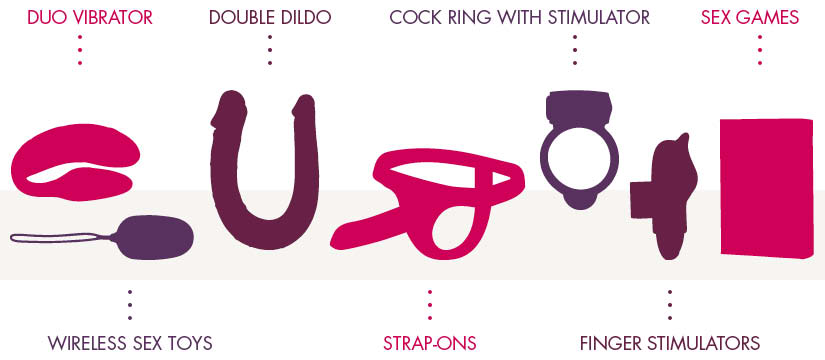
If you like compact, low-effort accessories once you’re fully healed, a palm-sized external vibe can add gentle warmth without friction; just start on low and keep consent first. Here’s a calm, consent-forward explainer for a pocket-friendly option you can bookmark for later: pebble sex toy. (Internal link included once.)
Clear answers to common questions (FAQ)
How long to wait for sex after yeast infection treatment if I used a 3-day cream?
Finish all three doses, wait until all symptoms are gone, then give yourself 2–3 days of buffer before sex. Remember that many vaginal creams are oil-based and can weaken latex condoms during treatment and shortly after—check your product insert and use non-latex barriers or abstain until you’re past the caution window. CDC+1
How long to wait after a single oral fluconazole tablet?
Many clinicians recommend waiting about a week, and only if you’re symptom-free. Symptoms usually start improving within 24–72 hours, but tissues still need calm time. GoodRx+1
Can I have sex if I still have mild itching but it’s “much better”?
Best not. Any lingering symptom means inflammation is present, and friction can set you back or re-irritate tissues. Wait until zero symptoms. Medical News Today
What about oral sex—same wait?
Yes. Wait until symptoms are gone and treatment is complete. Oral-genital contact can be linked with some yeast cases; let tissues fully recover first. Mayo Clinic
Do we need to treat my partner, too?
Not usually for uncomplicated infections. Partners who develop symptoms (e.g., balanitis) should be assessed and may need antifungals. Otherwise, routine partner therapy isn’t supported. CDC
Can I rely on condoms during treatment?
Use non-latex options or abstain during intravaginal azole therapy; many creams/suppositories weaken latex condoms and diaphragms. Check your label for exact timing. CDC+1
Is it okay to use lube when I’m healed?
Yes—prefer water-based (condom-compatible). If you’re sensitive, choose unscented, glycerin-free formulas and patch-test on inner arm first.
I keep getting yeast infections after sex. What now?
See a clinician. Recurrent VVC (≥3 in <12 months) often needs longer initial therapy and sometimes maintenance dosing after culture-guided testing. CDC
How do I know if it’s not yeast?
BV, trichomoniasis, dermatitis, and UTIs can mimic yeast. If OTC treatment fails or symptoms return quickly, get tested rather than guessing. CDC
I’m pregnant—any special rules?
Yes. In pregnancy, topical azoles for 7 days are recommended; oral fluconazole is not advised. Always check with your obstetric provider, and wait until symptoms are fully resolved before sex. CDC
Bottom line you can trust
For how long to wait for sex after yeast infection treatment, do this:
- Finish the full regimen.
- Wait until every symptom is gone.
- Add a small buffer (generally 2–3 days after your final vaginal dose, or about a week after a single oral dose).
- Protect condoms by avoiding latex with oil-based creams/suppositories during treatment (and per label afterward).
- If symptoms persist, return, or you’re unsure—see a clinician.
Give your body that extra bit of time. The payoff is faster healing, fewer setbacks, and a way better return to intimacy.


![Most Powerful Bullet & Mini Vibrators [Tested in 2025]](https://couplepleasure.com/wp-content/uploads/2025/10/image-11-2.jpeg)
